Home-based acute care services gaining foothold in Massachusetts
Providing acute hospital care services to patients in their homes is far from a mainstream practice, but the COVID-19 pandemic and changes to federal reimbursement practices may be accelerating efforts to expand these offerings in Massachusetts.

Eric Alper, M.D.
For example, UMass Memorial Medical Center in Worcester will admit its first hospital-at-home patients shortly, starting with about five patients and gradually growing the program to a census of 20, 30 or perhaps 50 over the next 6-to-12 months, depending on demand and staff availability.
According to Eric Alper, M.D., Chief Quality Officer and Chief Clinical Informatics Officer at UMass Memorial Health, the hospital was planning its program last fall when the Centers for Medicare and Medicaid Services (CMS) announced it would begin reimbursing these services on a par with inpatient care through a special waiver process. “That kind of pushed us over the edge to actually make a commitment to do it,” Dr. Alpers says.
UMass Memorial was not alone in taking advantage of the opportunity. Since November 2020, CMS has approved 147 hospitals across 32 states to participate in Acute Hospital Care at Home.
Lessons from existing programs
A number of organizations, including Boston’s Brigham Health and Massachusetts General Hospital, were already testing the efficacy, safety and potential cost savings of providing acute care services at home using other sources of funding.

Ryan Thompson, M.D.
Now in its fifth year, Massachusetts General’s Home Hospital currently serves about 25 patients per month and plans soon to expand the number and type of cases in the program, according to Medical Director Ryan Thompson, M.D. Patients with heart failure, pneumonia, chronic obstructive pulmonary disease and infections of the skin and urinary tract currently account for approximately 75% of Home Hospital’s cases, he says.
Dr. Thompson thinks most hospital departments have patients who could receive acute care services at home and mentions pediatrics as one example of a natural fit. “Just think of the benefit to parents and families from keeping younger, acutely ill patients at home,” he says. “We are not there yet, but as the field grows, I think pediatrics should absolutely be in our future.”
Most admissions for hospital-at-home services come through emergency departments and observation units, but some patients are admitted directly from home, ambulatory or urgent care centers, allowing them to begin treatment without delay. Dr. Thompson says these “upstream” admissions at MGH have been beneficial to patients but are not currently covered by the CMS waiver, which allows reimbursement only for patients admitted from the emergency department or transferred from an inpatient unit. “CMS is being appropriately cautious in limiting admissions to those settings,” he says. “However, our experience is that certain acutely ill patients can be admitted to Home Hospital directly from home or clinic so long as they are carefully evaluated and deemed appropriate for our service. Safely avoiding a busy emergency department can be a win-win for both patient and hospital.”
James Parris, M.D., Ph.D.
Operating under a different payment model affords the Veterans Administration Healthcare System more flexibility. James Parris, M.D., Ph.D., Medical Director of the Hospital in Home program at VA Boston Healthcare, explains the benefits of keeping acutely ill patients enrolled as they transition to subacute care. The program can also gradually reduce the number of medical specialists making in-home visits to every other day, every third day, etc., prior to discharge, with careful attention paid to how the patient is responding to care and assuming responsibility for self-management.
Safety gains described
Dr. Parris and others describe a number of safety gains that stem from treating patients in their own homes. For example, the pharmacist and nurses who do most of the home visits can see firsthand that patients often need help managing medication regimens. Dr. Parris, who also practices in palliative care and hospital medicine, notes that in traditional inpatient care, clinicians often don’t know how well patients are managing medications at home. He admits, “I was kind of blind to the idea that medication reconciliation at admission and discharge can be trivial compared to what you find when you see for yourself what’s in people's cupboards.”
In addition to medication safety, hospital-at-home programs are seeing reductions in falls, infections, delirium and readmissions. While the evidence base for these programs is still developing, a recent study of Brigham Health’s Home Hospital program demonstrated lower costs, fewer readmissions and less use of services such as imaging. Home Hospital patients were found to be more physically active than the inpatient control group. Increased activity, however, may increase the risk of falls, so frailty is important to include in pre-admission assessment. Dr. Thompson reports that MGH’s Home Hospital program follows the hospital’s best practices for safety for inpatients and closely liaises with the MGH Center for Quality and Safety.
Access concerns
Some hospital-at-home programs augment in-person clinical visits with remote monitoring and telemedicine, with required devices and connectivity provided by the hospital. At UMass Memorial, acute-care patients at home will be provided with all the necessary medical monitoring devices, a tablet to use for telehealth visits, and a cellular hot-spot. The technology vendor provides some workflows in Spanish, and Dr. Alper reports that UMass Memorial is working on including language interpreters by video. “Equity is something we're very sensitive to, not only from a language perspective, but also race, ethnicity and socioeconomic factors as well,” he says. “We want to make sure that patients are safe, our staff is safe and that we provide an equitable experience across the board. We will be actively tracking that as we get started with the program.”
Programs must also make sure that patients and other members of the household are comfortable with having clinicians come into the home on a regular basis.
Despite uncertainty, programs are optimistic about the future
Cost reduction was an original driver of testing the viability of providing services at home to patients who would otherwise be hospitalized. Prior to the CMS waiver, the programs at Brigham Health and MGH were funded largely as population health initiatives, according to Dr. Thompson.
Currently, CMS’s Acute Hospital Care at Home program operates with a waiver tied to the federal Public Health Emergency issued in response to the pandemic. The PHE is expected to be in effect at least through the end of 2021.
Dr. Alper expressed confidence that the trend toward alternative models of care will continue. Noting that a variety of value-based care models are in use and developing good track records, he believes the services are likely to remain eligible for reimbursement by CMS and ultimately other payers, although he admits the future is a bit uncertain. “To stay competitive and relevant to your patient population, you need to innovate and sometimes that involves taking a leap of faith,” he notes.
Dr. Thompson also believes that hospitals will need to offer more home-based care to stay competitive and that payers will recognize that the care model is cost effective, as some have already done. He looks forward to the day when hospital-at-home is seen as a first choice for patients, not an “alternative” pathway. “We should be doing all we can to grow these programs, to keep them full and to only admit to the hospital when we don't have any other option,” he says.
The Hospital at Home (HaH) Users Group is a collaborative for sharing resources and best practices. The group also plans to help develop standards to inform regulatory and reimbursement policies to support program expansion.
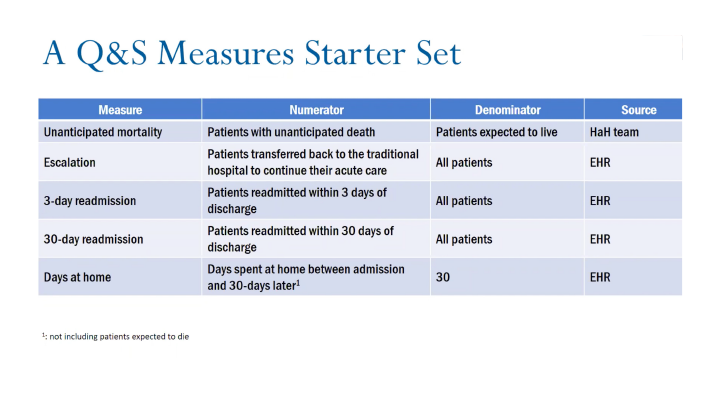
In addition to co-leading the Home Hospital program at Brigham Health, David Levine, M.D., is a founding leader of the HaH Users Group. A webinar he presented about evaluating safety and quality, “How Are We Doing?” is available on the group’s website. Dr. Levine suggests adding three measures to those required by CMS (in addition to patient volume) to form a starter set of five quality and safety measures for HaH programs.