A coordinated effort is key to stemming sepsis
With the formation of a statewide Sepsis Consortium this year, Massachusetts joins the ranks of states across the country that are developing new strategies to prevent the devastating effects of sepsis on patients and families.
Sepsis is an inflammatory response to an infection, which overwhelms the body; it can lead to a host of debilitating health problems, including organ failure and death. If caught early, sepsis can be treated. Although it is the leading cause of death in U.S. hospitals, sepsis isn’t well understood. It can originate as an infection acquired during a hospital stay, but can also get its start in an uncleaned wound from a scraped knee on the playground or a case of the flu. The progression from infection to sepsis can vary widely.
To improve awareness, prevention, diagnosis, treatment and health outcomes, a number of states across the country have recognized the need to address sepsis by engaging participants from many disciplines and populations. This includes health care providers, the public, and government agencies.
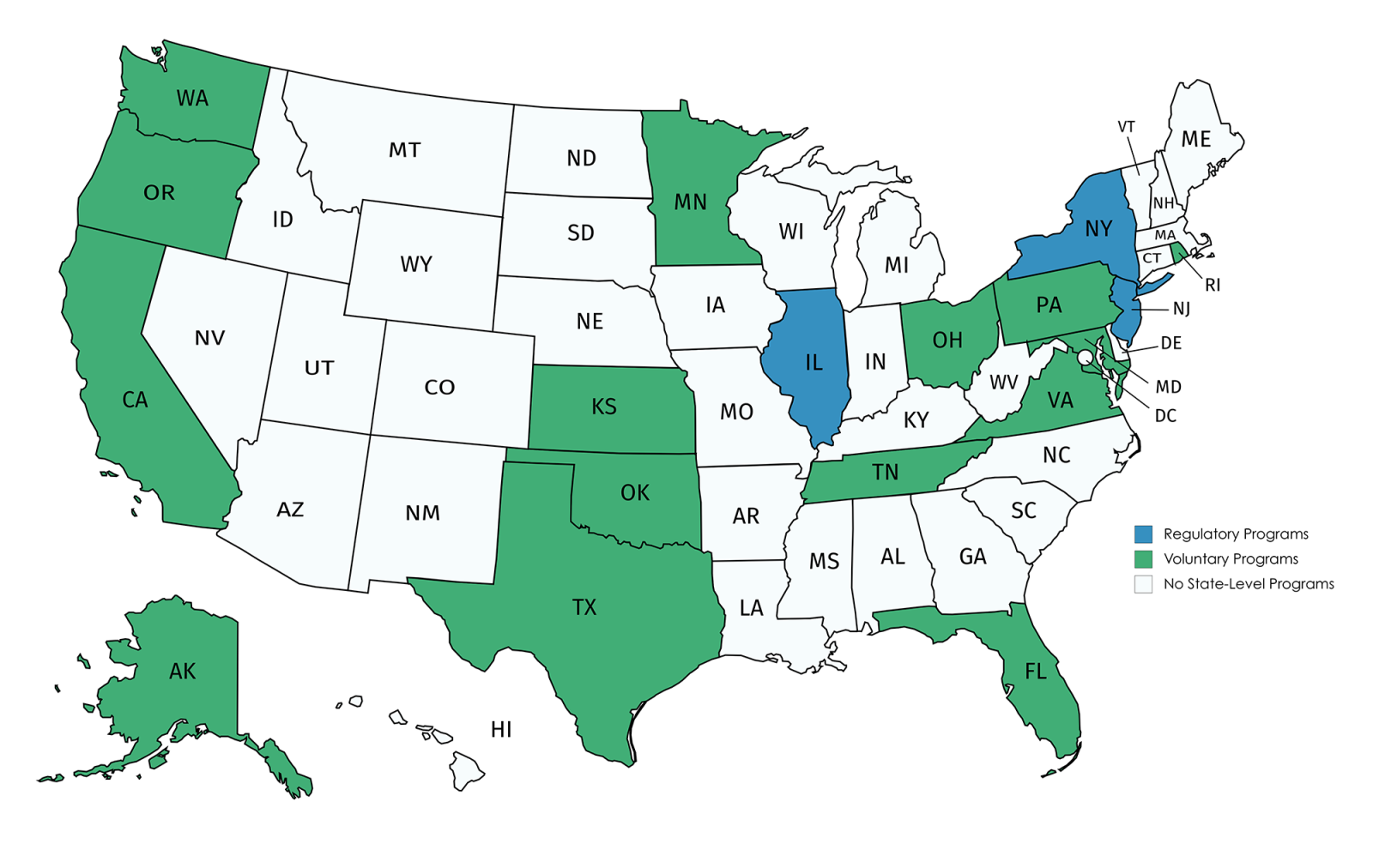
The Betsy Lehman Center completed a review of sepsis programs in all 50 states and found that 18 states have coordinated sepsis programs. Of these 18, we found that 15 are using collaborative approaches, mostly among hospitals. Three other states, Illinois (2016), New Jersey (2018), and New York (2013) leveraged statutory or regulatory power to try to make sepsis recognition and management more uniform in hospitals across the state. New York also mandated education programs for school-aged children to boost awareness of the early signs of sepsis.
In Massachusetts, sepsis is a leading cause of hospital admissions, second only to labor and newborn delivery. The new Consortium will provide strategic direction for a meaningful, statewide response to sepsis to address the high cost of sepsis to patients, families and the health care system.
That response will include a collaborative effort to ensure that every Emergency Department in the state implements an evidence-based protocol for rapid, effective diagnosis of sepsis, as well as a campaign to educate a broader group of health care providers and the general public about the symptoms of sepsis and the need for urgent action.
To learn more about other states’ efforts that are informing Massachusetts’ approach, read this brief report from the Betsy Lehman Center summarizing sepsis initiatives across the country and lessons learned.