A new framework to address diagnostic error during COVID-19

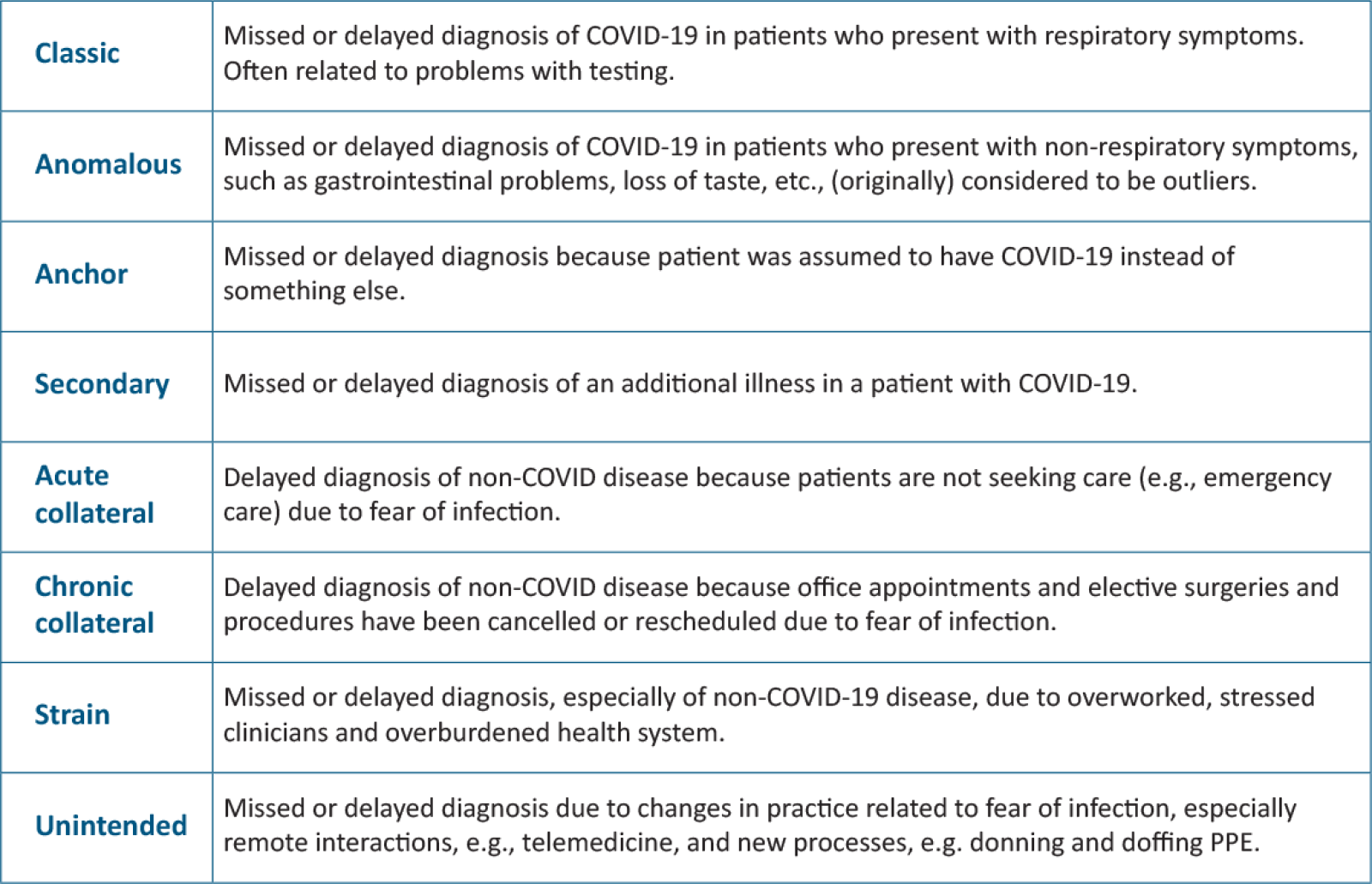
In the context of COVID-19, Tejal Gandhi, M.D., and Hardeep Singh, M.D., offer a new framework for addressing diagnostic error. The new "typology" includes eight categories ranging from "classic" risks associated with testing problems and "strain" related to working in stressful conditions to "chronic collateral" risk from screening that was delayed while most medical facilities were closed to all but patients with urgent needs because of the virus.
Dr. Gandhi, Chief Safety and Transformation Officer at Press Ganey in Boston and Dr. Singh, Chief of the Health Policy, Quality & Informatics Program at the Center for Innovations at the Michael E. DeBakey VA Medical Center in Houston, say the errors "span the entire continuum of care and have both systems-based and cognitive origins."
Dr. Gandhi says there is an urgent need to recognize and address diagnostic problems in real time. “It’s important to begin moving into solutions while also determining how to capture diagnostic error events. We don't want to spend six months designing the perfect mechanism for identifying events and lose that time in terms of prevention,” she says.
COVID-19 also demands that organizations accelerate implementation of proven solutions. Gandhi notes a common assumption that culture change — an important driver of patient safety improvement — is slow and says it doesn’t have to be: “There are things leaders can do today. Physician leaders, for example, can acknowledge that diagnostic errors happen and start talking about it with colleagues. Transparency, openness and helping people feel comfortable talking about these kinds of errors can happen tomorrow in organizations. That's the first step.”
As medical practices and hospitals start to offer non-urgent services again, they face a number of challenges, including how to prioritize scheduling patients whose appointments, screenings, surgeries, wellness visits and more were postponed.
Dr. Gandhi encourages practices to be mindful of disparities in health care, including diagnosis, when planning for patients’ care needs in the coming weeks and months. Some racial and ethnic groups have been disproportionately affected by COVID-19, and many communities of color include patients who have been chronically underserved. Gandhi says, “One of the big questions related to diagnosis is how you prioritize who comes in first and how to think about patients who may be at higher risk. We also need to ensure that that we're not focusing only on certain populations, and we have to constantly be looking for where we may be unintentionally widening the gaps.”
Diagnostic error nomenclature for COVID-19
Primary-care Research In Diagnosis Errors, a Boston-based network that examines missed or delayed diagnosis is soliciting cases of misdiagnosis related to COVID. If you know of a case to share for further study and discussion, click on “Submit a case” on this page.