'Equity bundle' aims to reduce racial and ethnic disparities for birthing families
More than half of all Massachusetts birthing hospitals are participating in a nationwide effort to reverse the significant rise in adverse events and outcomes among all people giving birth and reduce racial and ethnic disparities.
The Perinatal-Neonatal Quality Improvement Network of Massachusetts (PNQIN) is currently working with 22 hospitals — and enlisting others to join — to track and prevent inequities in maternal health outcomes. This work is part of a national safety initiative organized by the Alliance for Innovation on Maternal Health (AIM) to “make birth safer, improve maternal health outcomes and save lives.” PNQIN provides guidance, education and technical assistance to Massachusetts hospitals participating in the initiative.
According to a recent study, the rate of serious maternal complications from labor and delivery has risen for all racial and ethnic groups in Massachusetts. Black pregnant people, in particular, are more than twice as likely to experience serious complications than their peers who are white. The study measured severe maternal morbidity (SMM) across more than 1.5 million deliveries between 1998 and 2018. SMM reflects unexpected complications from labor and delivery that result in short- or long-term consequences for the health of the person giving birth.
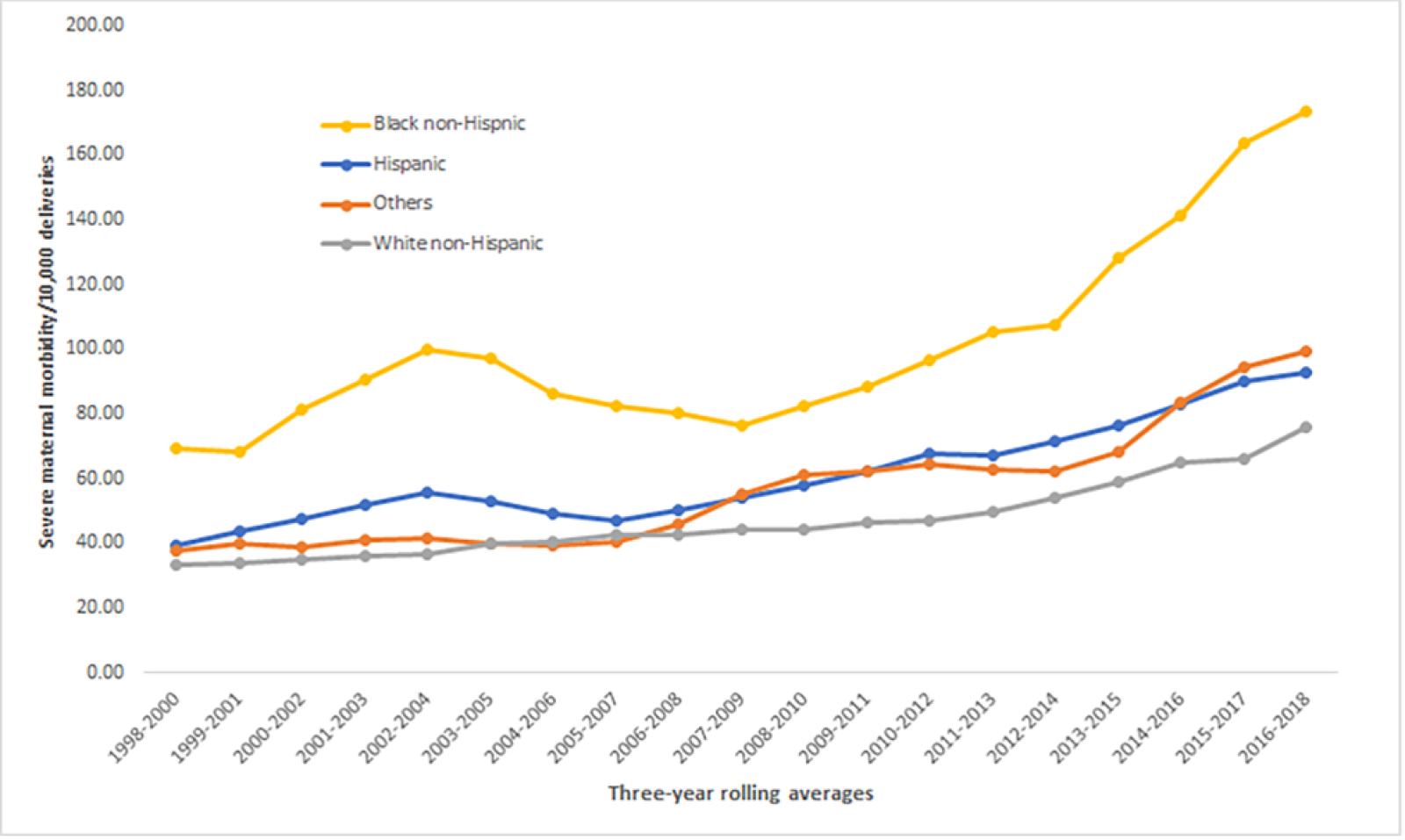
Severe maternal morbidity by race and ethnicity in Massachusetts, 1998–2018.
PNQIN's Maternal Equity Bundle, based on AIM’s maternal equity framework, offers hospitals and other providers a series of best practices that can be used to improve outcomes for people of color during pregnancy and childbirth.

Audra Meadows, M.D., M.P.H.
Audra Meadows, M.D., M.P.H., Lead for PNQIN’s Maternal Equity Bundle, says, “It’s exciting to have this work moving forward across Massachusetts. Our ultimate goal is to support birth hospital teams in ensuring perinatal quality and excellence for all, which means we need to look at outcomes for sub-populations by race, ethnicity, language, etc., to support their needs for an optimal birth experience and outcome.”
Components of the initiative address organizational systems, staff member and provider actions, and patient and family interactions. Examples of best practices include routinely and accurately documenting each patient’s self-identified race, ethnicity and primary language and providing a way for patients, families and staff to report inequitable care and episodes of miscommunication or disrespect. Clinical units are directed to build a culture of equity, including systems for reporting, response and learning, similar to ongoing efforts in safety culture.
AIM also promotes improving care for people giving birth with patient safety bundles for obstetrical hemorrhage, severe hypertension, reduction of cesarean birth, cardiac conditions, substance use disorder, postpartum discharge transitions, perinatal mental health conditions and sepsis.
The bundles include actions that are evidence-based and adaptable for use in a variety of settings and resource levels. When performed collectively and reliably, they have been shown to improve patient outcomes.
AIM’s initiatives are supported by the American College of Obstetricians and Gynecologists, the American Hospital Association, the American College of Nurse-Midwives and other AIM partners. AIM is funded by the Health Resource and Services Administration of the U.S. Department of Health and Human Services.
The Betsy Lehman Center serves as a data repository for hospitals using PNQIN’s maternal equity bundle. Seventeen hospitals in Massachusetts have submitted data since October, when the bundle was launched, and PNQIN leadership expects the number to grow in the coming months. The Betsy Lehman Center is also collecting and analyzing maternal health outcome data on behalf of PNQIN to track the state’s progress on reducing inequities and to help individual hospitals compare their progress to their peers in the state.
PNQIN’s spring 2023 summit in April offers an opportunity for hospitals to learn more about collaborative, equity-focused efforts.
Participating facilities can turn to TeamBirth for support
In Massachusetts, some hospitals are also turning to TeamBirth for support as they put the equity bundle into practice. Led by Ariadne Labs, TeamBirth facilitates shared decision-making through structured and planned communication between the patient and members of the care team, including the physician, midwife, nurses and other patient support personnel.

Amber Weiseth, R.N., D.N.P.
The TeamBirth approach is flexible, adapting to the needs of participating hospitals. The team from Ariadne typically works with a cohort of seven to 10 hospitals to provide training and guidance in preparation for implementing the care model. TeamBirth facilitators will also meet individually or in small groups with subsets of the cohort, such as unit leaders at a birthing site, to help them tailor the information to their community’s needs.
Amber Weiseth, R.N., D.N.P., Director of Ariadne’s Delivery Decisions Initiative, says, “When fully implemented, TeamBirth is a powerful way for people giving birth to routinely be at the center of their care. We strive to make the right thing — including patients in decision-making and honoring their choices — the easy thing to do.”