A nursing shortage had been building in Massachusetts for more than 10 years when COVID-19 shocked the system in early 2020, triggering a dramatic increase in the number of vacancies across all health care settings. Generational change, regional demographics and economic factors are contributing to the undersupply of nurses that is expected to last for years.
Nurse leaders, hospital and post-acute care executives and other industry experts discussed innovative actions to address immediate and future challenges in the nursing workforce at a half-day virtual conference held by the Massachusetts Health and Hospital Association (MHA) and the regional Organization of Nurse Leaders (ONL) on October 19, 2021.
Before the pandemic, the shortfall of all health care professionals in the state was projected to more than double from 19,000 in 2019 to 43,000 in 2024, according to the Massachusetts Executive Office of Labor and Workforce Development. At the MHA/ONL event, Jennifer James Price, the agency’s Undersecretary for Workforce Development, said that issues related to the staffing shortage, including delays in care and higher labor costs “have been fully exacerbated by COVID. It’s been a massive shock to our economy and workforce.”
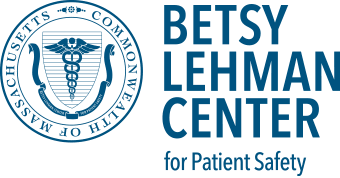
The most recent statewide data is from 2019 when 6.4% of registered nurse positions were vacant, representing 1,409 unfilled positions. Those figures come from an annual survey conducted by MHA and ONL since 1988. On October 19, MHA ‘s Executive Director and Chief Data Officer, Anu Puri, M.D., characterized the 2019 staffing data as “prehistoric,” given the disruption that COVID-19 delivered to the system overall and nurse staffing in particular.
Dr. Puri said that this year’s version of the annual staffing survey, which will be distributed to hospitals shortly, will help assess the impact of the pandemic with new questions about the use of travel and agency nurses, suspension of RN clinical practicums, the effect of staff vaccine mandates and more.
The details of the current staffing crisis continue to change as more people become fully vaccinated against COVID-19 and the number and nature of hospital admissions evolve. Massachusetts cases of COVID-19 are currently down from their earlier highs, but more patients are seeking care for delayed medical needs, and hospitals continue to operate at or near capacity.
Retention is also key to adequate staffing
While responding to the current staffing crisis, nurse leaders are also focusing on recruiting and retaining new nurses for the future. In addition to actions such as sponsoring high school job fairs and helping associate degree nurses advance toward bachelor’s degrees while also practicing, organizations may need to examine several well-known drains on nurses’ time, such as hunting for supplies or entering data, experts say.
Speaking at the MHA/ONL event, Marsha Maurer, R.N., D.N.P., Senior Vice President for Patient Care Services and Chief Nursing Officer at Beth Israel Deaconess Medical Center, spoke about the need for professional development in nursing. The concept of productivity should be reframed to include activities that support providing high-quality patient care, such as graduate education and research, even if that time is not spent in direct patient care, she argues. Within the profesion, nurses and nurse leaders may similarly need to re-examine what being a nurse involves, especially as the demographics of the workforce change.
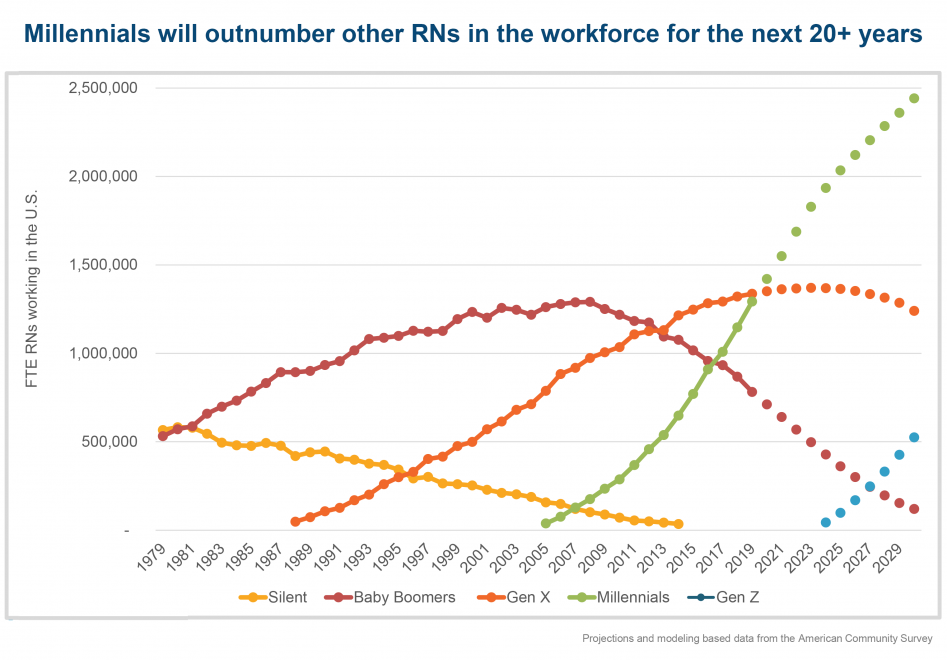
At the same event, Nancy Gaden, R.N., D.N.P., Senior Vice President and Chief Nursing Officer at Boston Medical Center, reported that in one department at BMC, all of the newly graduated nurses hired last year have now returned to school to work on advanced degrees. Gaden says, “We’ve got to get through this crisis, look five years down the road and create a workplace that’s exciting for that group of millennial nurses who are looking for something different.”
The number of millennials — individuals born between 1982 and 2000 — working as nurses in the United States has grown rapidly since the mid-2000s, when they began to enter the workforce. Based on research he is doing at the Interdisciplinary Center for Workforce Studies at Montana State University, David Auerbach, Ph.D., projects that, having equaled the number of nurses in the preceding “Generation X” in 2020, millennials will greatly outnumber other nurses for the next 20 years. Dr. Auerbach is also Senior Director for Research and Cost Trends at the Massachusetts Health Policy Commission.
Maurer observed that reframing productivity in nursing is part of making the case to non-nursing executives and board members for a new kind of investment in this critical workforce. “We have to make the case that an investment in lots of different kinds of productivity — direct patient care, producing research, educating future students; all those things are productive,” says Maurer. “We need to make all of this visible. People are very habituated to a different frame. We need to get the word out to our colleagues and our boards.”