MHA’s Vice President of Health Equity reports progress on the state’s equity-focused Medicaid waiver

Isabelle Lopes, M.S.W., M.P.H.
Isabelle “Izzy” Lopes, M.S.W., M.P.H., is Vice President of Health Equity at the Massachusetts Health & Hospital Association where she is helping hospitals meet requirements of the state’s newest Medicaid waiver. Lopes is a member of the Health Equity Compact and serves on the Betsy Lehman Center’s Health Care Safety Education and Curriculum Advisory Committee. She holds master’s degrees in social work and public health from Boston University and is pursuing a law degree at Suffolk University Law School.
Patient Safety Beat: The Medicaid waiver has been in effect since January of 2023, and hospitals have already met the initial goals of its Hospital Quality and Equity Incentive Program. Please describe some of the current and upcoming goals.
Izzy Lopes: The waiver is a monumental program — $2.2 billion over five years to incentivize acute care hospitals to improve equity and reduce health disparities. The state assesses hospitals for roughly half of the funding, which is matched with federal money. Hospitals regain those funds by reaching specific health equity goals.
From MHA's report, ONE YEAR IN: Massachusetts Hospitals’ Historic Health Equity Commitment
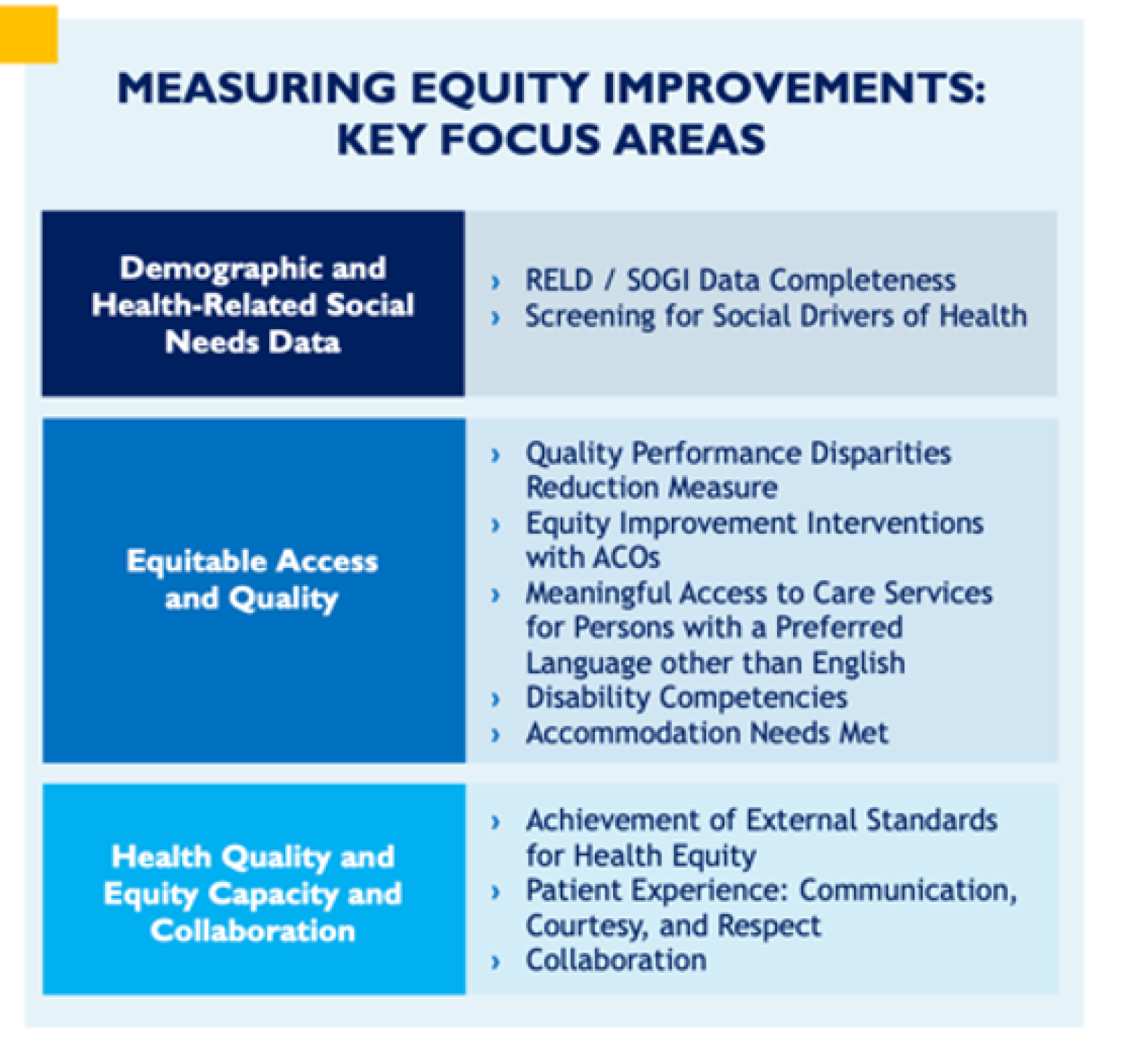
In 2023, the foundational year of the waiver, hospitals worked on infrastructure and submitted plans to MassHealth describing their strategy for addressing waiver elements. This year, hospitals are collecting patients’ demographic data, creating screening tools for health-related social needs, self-assessing language interpretation services and disability-competent care, and more.
It's notable that hospitals will be working toward attaining health equity certification from The Joint Commission. MHA expects all hospitals in the state to be certified by the end of 2025. The domains of The Joint Commission’s certification align closely with the waiver. It is an opportunity for hospitals to show they have met milestones that move them closer to eliminating health disparities and achieving optimal health outcomes for the patients they serve.
As we talk about the certification process and the waiver, I want to add a note of caution. This work requires “seeing the beyond,” looking to the future. Attaining certification or reaching the end of the waiver period won’t necessarily mean that health equity is achieved. We must make sure that our hospitals are appropriately positioned to continue this work beyond the life of the waiver. It is about building a solid foundation and sustaining the improvements that will advance health equity.
Patient Safety Beat: How do efforts to reduce health disparities relate to ongoing efforts to improve patient safety?
Izzy Lopes: The relationship is quite direct. We know, for example, that language barriers and cultural differences hinder effective communication between patients and providers. Miscommunication can lead to misunderstandings and errors. Initiatives aimed at increasing diversity among health care providers and promoting cultural intelligence and sensitivity can help.
We also need to pay attention to the issue of implicit bias and the way that unconscious attitudes and stereotypes may affect the perceptions, behaviors and decisions of providers, resulting in differential treatment.
The patient community is not a monolith. In addition to developing better cultural intelligence, developing a more diverse health care workforce will help improve safety. Receiving care from someone who looks like them helps patients trust their providers. It helps give patients confidence that someone is listening, hearing their story and understanding their experience. That allows for greater disclosure in terms of what the patient is experiencing at the time.
Health organizations must commit to examining the policies that may contribute to racial inequities. We know that systemic racism widens these gaps and makes care less safe for many patients.
In addition to implementing meaningful strategies to improve safety, we must couple these actions with humility. To do so, we must truly listen to these communities and elevate their voices and stories in the process.
Patient Safety Beat: In 2024, the waiver asks hospitals to screen inpatients for social determinants of health, including housing status, transportation access and food insecurity. How will hospitals use the data?
Izzy Lopes: As our hospitals ask patients these questions — Do you have access to food? Do you have safe housing? Do you have any unmet transportation needs? — they develop an understanding of the population, which allows them to create patient-centered interventions.
Having this data also helps hospitals build relationships with community-based organizations to address social determinants of health. If access to healthy food, for example, is an increasing concern for the patients you serve, that presents an opportunity to partner with an outside organization that provides such services. Those linkages are being forged on a regular basis by our hospital systems because they can see the data, ascertain patients’ needs and help provide services.
On a basic level, having reliable sources of healthy food or childcare or simply being able to get to the hospital are immediate needs that must be addressed. Patients will have trouble focusing on higher-order health concerns — things like A1C levels and hypertension control — if their immediate needs are not addressed first.
Ultimately, we must recognize that we are truly doing this for our patients. To elevate the voices, stories and lived experiences of the patients who our members serve, we need to know who they are.
Patient Safety Beat: Hospital leaders are working on many urgent, inter-related improvement goals, including patient experience, workforce well-being and retention, and health equity, which all affect safety. Do you see opportunities to link these workstreams into a more coordinated system of continuous improvement that “lifts all boats”?
Izzy Lopes: Keeping all of these interests in mind while creating a more coordinated system committed to continuous improvement requires hospital leaders to align many stakeholders around a shared vision of an equitable health care ecosystem. We must first ask: What is the system we want to create together?
We can link these work streams — equity, experience and workforce — which I like to imagine flowing together like a river, not as separate, distinct work streams, and create a more integrated care delivery system.
Ultimately, we must recognize that we are truly doing this for our patients. To elevate the voices, stories and lived experiences of the patients who our members serve, we need to know who they are. With better demographic information, we will learn how many patients are differently abled, what languages they speak, how they identify and more. That will enable hospital systems to assemble care teams and create infrastructure that takes patients’ unique needs and differences into account.
The same principle is at the core of creating a highly trained and skilled, interdisciplinary and competent workforce that reflects the population they care for. When we talk about the skills of the workforce, we’re looking beyond technical skills to the ability to understand cultural nuance and appreciate what patients are contending with in their lives, what challenges they face as they try to stay healthy.
Equity is the distinguishing feature of the waiver, which our hospital systems are approaching with great intentionality and commitment. Their passion is resonant and palpable as we hear them brainstorm ideas, talk about workflow and process, and share how they are supporting the workforce to be more culturally aware and attuned to the needs of their patients.