New research highlights home care workers’ views on safer care
COVID-19 has had a deep impact on the home care sector, exposing gaps in information, policies and protections that can lead to increased risk for members of the home care workforce and their clients, according to a new report from the Betsy Lehman Center for Patient Safety.
The report, “From the Frontlines: Home care workers voice COVID-19 challenges and ideas for change,” outlines key themes from focus group research with more than 80 members of the Massachusetts home care workforce. Workers described pandemic-related challenges to safety and offered ideas for improvement that could add stability to this vital sector of the health care continuum well beyond the pandemic. They urge greater attention to:
- Allocation of scarce resources, such as personal protective equipment (PPE) and testing for COVID-19;
- Informational needs, ranging from prompt notification of possible COVID-19 exposure to consistent infection control training that accounts for the unique nature of care delivery in people’s homes; and
- Workforce retention and burnout issues, including inadequate compensation and lack of respect for their work.

Participants also offered a number of suggested actions that would strengthen the home care sector, ranging from delivering consistent, targeted infection control training and guidance to providing structural incentives for workers to stay home when they might be sick.
Massachusetts residents are able to live in the community because of the services of over 100,000 home care workers, including personal care attendants, home care aides, home health aides, occupational therapists, physical therapists and other members of allied health professions.
Home care work involves close personal contact but the PPE during the pandemic has generally been limited to mask and gloves, the participants said. In many cases, they rely on cloth rather than medical-grade masks. Fewer than half of the participants typically used face shields or goggles, though 84% help with activities of daily living, such as bathing, dressing and oral hygiene for people with disabilities and older adults at high risk for complications if they contract COVID-19.
I actually carry around a letter that's dated from the state of Massachusetts, the Commonwealth, that states that I'm an essential worker. And I just feel good that somebody says, hey, what we're doing is important, it's essential, and we're going to recognize that.
Workers travel among apartments, homes, assisted living residences and nursing homes to provide care services raising both their risk of exposure to COVID-19 and spreading it to the people for whom they care. More than 60% of the focus group participants provide services to two or more people in the same day, with almost half of that group working with five or more clients on a typical day.
Home care workers worry about getting COVID-19 on the job and nearly 1-in-3 considered leaving home care work because of conditions brought on by the pandemic.
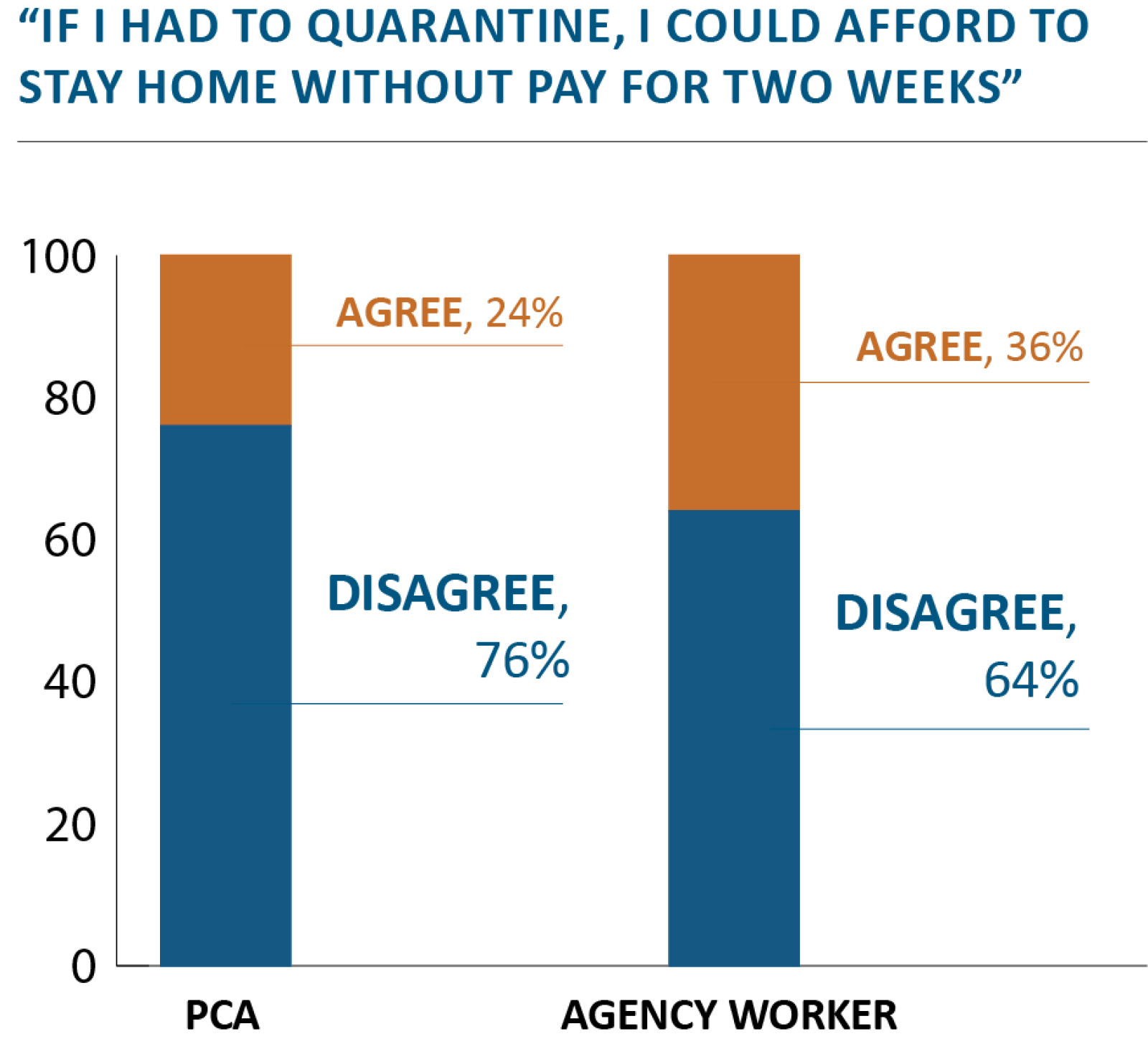
Asked what they or their colleagues would likely do if they thought they may have been exposed to the virus at work, participants described the dilemmas they face. “If it was simple, [a potentially exposed worker] should just stay home and get tested for COVID and not expose any other clients in case it is COVID. But that said, I think it is not that simple because not everybody has the money to do that and you also care about your clients. But I think that when you need the money and you don’t know if you are sick, you don’t want to take the chance of staying home for nothing,” one worker says.
Home care workers also have little control over the home environments in which they work. “You could have a patient that has, like, six kids and grandchildren and they all have come to visit during the week. Or … or it could be the opposite — none have come to visit, you know? You just never know,” one worker says.
Another adds, “Our agency is affiliated with a hospital and so in the hospital, you can’t walk in without a mask or a face shield, you can’t have visitors. In home care, I can ask my clients and their families to put a mask on and if they say ‘no,’ I’m not allowed to leave. I still have to stay there and provide care. That doesn’t make any sense to me.”
Instead, they try to manage situations as best they can, often relying on the relationships with the people they care for.
“I see like 30 patients a week and none of my patients or any in their family have gotten sick and nobody at my house has gotten sick and I think that’s because me and my clients, I’ve had them for a while, we’re kind of on the same page. We appreciate helping each other, you know what I’m saying?”
The focus group research, which follows a report issued late last year in partnership with the Safe Home Care Project at the University of Massachusetts-Lowell surveying home care agencies in the state, is part of a larger effort to better address the safety needs of the home care sector, according to Betsy Lehman Center Executive Director Barbara Fain.
We haven't left the patients isolated. I am proud that I have continued to show up despite the chaos and risks.
“Home care is a vital service for so many, yet it is often seen as something that is on the periphery when we think about health care delivery in the state,” she says. “These services can improve quality of life for people and their families while also relieving pressure on other more intensive health care settings. It is integral to the continuum of care and needs to be accounted for and prioritized when making policy decisions and allocating quality improvement resources.”
The Center conducted the focus groups virtually in October and November of 2020 using Zoom. Participants included 39 personal care attendants and 44 workers affiliated with home care agencies. The Center was able to recruit only seven people who receive home care services. The perspectives of home care client and consumer-employers also would inform program or policy changes to strengthen this sector.
Despite the challenges, workers expressed pride in what they are able to do each day.
“ … I actually carry around a letter that’s dated from the state of Massachusetts, the Commonwealth, that states that I’m an essential worker. And I just feel good that somebody says, hey, what we’re doing is important, it’s essential, and we’re going to recognize that,” one participant says.
Another adds, “We haven’t left the patients isolated. I am proud that I have continued to show up despite the chaos and risks.”
PCAs receive first dose of COVID-19 vaccination at a clinic on January 24, 2021.
Photos courtesy of 1199SEIU United Healthcare Workers East
Related content
Hospitals should partner with home care workers, Commonwealth Magazine (February 2021)